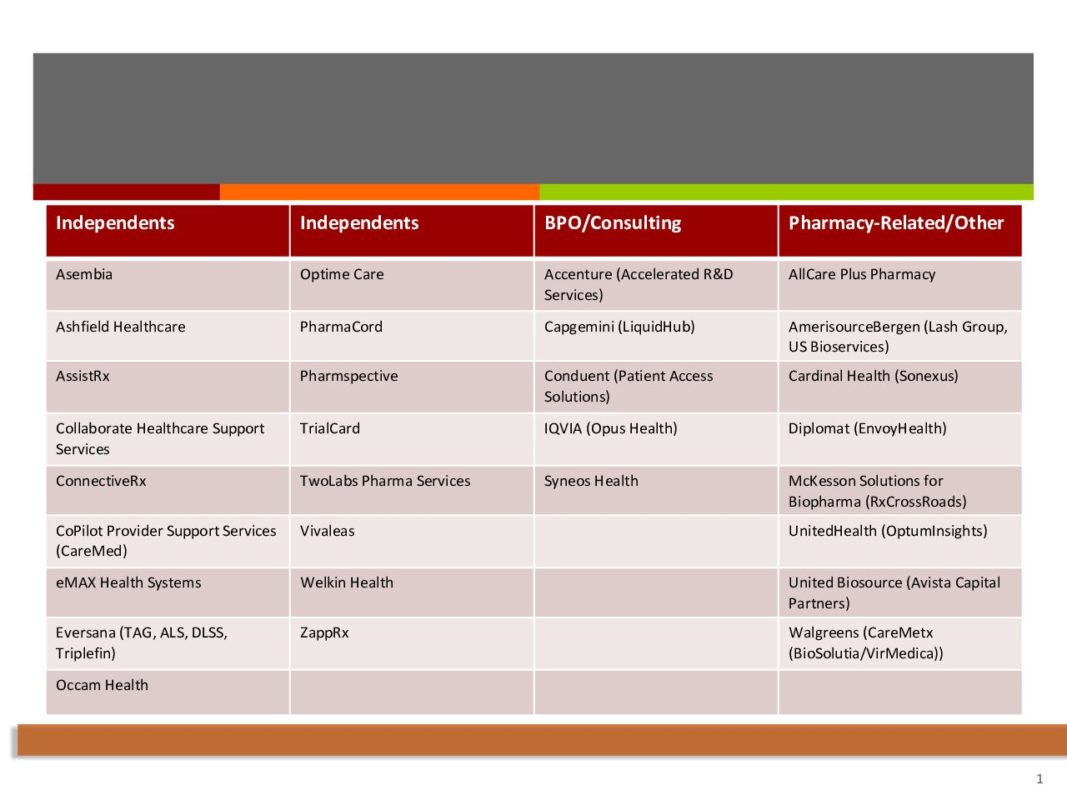
Specialty Pharmaceutical Hub Services Providers 2019 Report
Always Be a Step Ahead
Learn the important healthcare trends that could affect you in advance. Get expert analysis and discover the innovative ideas that are helping businesses overcome today's challenges.
Subscribe to AMI's Insights Newsletter Today.